We know that our intestines contain a large number of richly diverse bacteria that form their own ecosystem. This “gut microbiome” is now recognized to be an organ in itself and a rather important one at that.
The good bacteria in our gut help us fight diabetes, break down environmental toxins like pesticides in our food, and detox our bodies. Moreover, there is increasing evidence now that these little bugs even have a say in how we respond to therapeutic drugs.
Think of this the next time you pop a pill!
How Gut Bacteria And Medicines Interact
Drugs taken orally pass through the digestive system into the large intestine, the home of the microbiome and the site of complex drug-microbial interactions. Medicines like antibiotics are well known to alter the intestinal microenvironment and disrupt the population balance of gut bacteria.
At one time, metabolizing drugs was thought to be the job of large organs like the liver, which turns chemical compounds into water-soluble molecules that are easier to absorb or eliminate. Now, gut bacteria are also implicated in how effective a drug can be. The gut bacterial composition can even be the culprit when certain drugs, life-giving to some, cause severe toxicity in others. Gut microbes can even influence how cancer patients respond to immunotherapy.
What Is Pharmacomicrobiomics?
The last decade has birthed a new field of study called “pharmacomicrobiomics.” Despite its tongue-twister of a name, basically, it investigates the complex interactions between the gut microbiome and the drugs ingested by the host: how they are absorbed, distributed, metabolized and excreted from the system.
Enzymes and other molecules associated with gut bacteria influence how certain medications are activated or broken down. Hardly is it more evident than in the case of the drug Levodopa (a.k.a L-dopa) used to treat the motor symptoms of Parkinson’s Disease, which trace back to a scarcity of the neurotransmitter dopamine.
Researchers were curious as to why some individuals respond so well to this drug, and why it has little to no effect on others.
L-dopa is given along with a protective compound, “Carbidopa” which prevents it from being broken down before it reaches its target organ, the brain, where L-dopa is converted into dopamine. Despite that, the actual amount of L-dopa that makes it to the brain varies greatly among patients. As it turned out, certain patients were found to host gut microbes that override Carbidopa and sponge up the L-dopa well before it reaches the brain.
Studies also showed that Parkinson’s patients who have higher levels of a bacterial-origin enzyme, tyrosine decarboxylase, require higher doses of L-dopa to control their symptoms. This is because the chemical reaction this enzyme brings about is the same one that converts L-dopa to dopamine. Dopamine, once formed, cannot cross the blood-brain barrier, but L-dopa can, and needs to.
So one solution might be for these patients to increase their dose of L-dopa so as to retain sufficient amounts that finally make it to the brain.
The Good Side Of Things

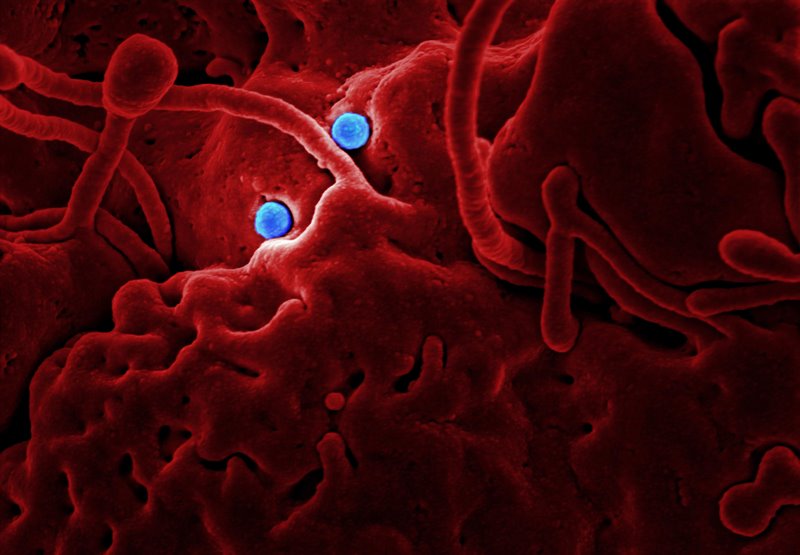
Image by Digbi Health
On the plus side, certain drugs are helped along by the byproducts of their interaction with gut bacteria. For example, an oral antibiotic sulfasalazine is ineffective until gut bacteria metabolize it. Metformin, the first-line medication for Type 2 Diabetes, somehow alters the gut microbial population in ways yet unknown, which actually increases its efficacy!
The Road Ahead
Findings like these really underline the need to further study the gut microbiome and specific genes that influence the drug response. Such research would be the essential first step to identify biomarkers that can guide doctors in prescribing drugs that are the most effective, and the safest, for individual patients.
Pharmacomicrobiomics could well set a new benchmark for personalized medicine.
Trials are already underway to test probiotic formulations or fecal transplants aimed at improving cancer immunotherapy outcomes.